
The Bhamashah Swasthya Bima Yojana is a flagship health insurance scheme launched by the Government of Rajasthan to ensure cashless, quality healthcare services for the economically vulnerable sections of society. By covering a wide range of medical and surgical treatments across empanelled government and private hospitals, Bhamashah Swasthya Bima Yojana aims to reduce the financial burden of hospitalisation on poor families. The scheme primarily benefits families listed under the National Food Security Act (NFSA) and those holding valid Bhamashah or Jan Aadhaar cards, making healthcare accessible and affordable to millions across the state.
What is Bhamashah Swasthya Bima Yojana?
Table of Contents
Bhamashah Swasthya Bima Yojana is a health insurance/health scheme by the Government of Rajasthan, aimed at providing cashless health care/hospitalisation facilities to economically weaker families.
Under this scheme, eligible families get hospitalisation treatment—which includes a defined number of medical/surgical packages—in empanelled hospitals, both government and private.
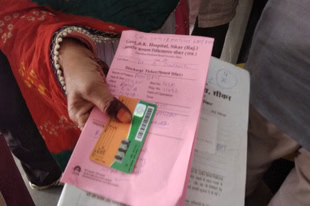
It is linked with the Bhamashah Card system, which is a state‑ID / beneficiary card in Rajasthan, often issued to the female head of the household, used for government welfare scheme identification.
Eligibility Criteria For Bhamashah Swasthya Bima Yojana:
To get benefits under Bhamashah Swasthya Bima Yojana, you must satisfy certain conditions. Key eligibility points:
Resident of Rajasthan: Must be a permanent resident of Rajasthan.
Bhamashah Card / Jan Aadhaar Card Holder: The beneficiary family must possess a valid Bhamashah card or Jan Aadhaar card.
Included under the National Food Security Act (NFSA): The family should be listed as a beneficiary under the NFSA (priority households or Antyodaya families).
Socio-Economic Caste Census (SECC) 2011 Data: Families identified as economically vulnerable in SECC 2011 data may also be eligible.
Ration Card Holder (linked to NFSA): Must hold a valid ration card linked to NFSA entitlements and should have availed ration recently (often within the last 3 months) to ensure active status.
Income Criteria (if applicable): In some cases, families below a specified income threshold (BPL or similar) may qualify, especially if not covered under NFSA.
Valid Government Identity Proof: Must possess Aadhaar or other valid ID proof for identity verification.
Documents Required For Bhamashah Swasthya Bima Yojana:
Here are documents typically needed to apply or to avail treatment:
- Bhamashah card (or Jan Aadhaar / Bhamashah acknowledgement slip)
- Aadhaar card or other government‑issued identity proof
- Ration card (especially NFSA / Fair Price Shop ration card)
- Proof of residence (as required)
- Sometimes income certificate / socio‑economic survey listing or proof of inclusion in the NFSA list/welfare lists.
How to Apply For Bhamashah Swasthya Bima Yojana:
Here is the application/enrolment process:
Check if you’re eligible:
Use the eligibility criteria (residency, NFSA, Bhamashah card, etc.) to see if your family is in the beneficiary lists. You can check via Fair Price Shop NFSA reports, or via Bhamashah / Health department resources.
Obtain or ensure you have the necessary documents:
Make sure you have your Bhamashah card / Jan Aadhaar, Aadhaar or ID proof, ration card, etc. If any are lacking, complete those first.
Visit an empanelled hospital or health facility:
To avail treatment under Bhamashah Swasthya Bima Yojana, you need to go to a hospital that is under the scheme. At the hospital, there is usually a desk or staff member (sometimes called Swasthya Sahayak or similar) who helps with verifying eligibility.
Verification at the hospital:
Present your Bhamashah card / ID/ration card, etc. The hospital staff will verify your details via Aadhaar or other identity systems. They also check whether you are listed under the NFSA or relevant welfare list.
Admission / Treatment:
Once eligibility is confirmed, you can proceed to take treatment. The scheme provides cashless treatment for covered procedures (hospitalisation, etc.). Pre‑hospitalisation and post-hospitalisation costs are included as per defined rules.
Claim and billing:
The hospital will handle the claim process for covered treatments. You should not need to pay for items covered under the scheme in an empanelled hospital once everything is verified. The hospital forwards bills, etc., to the government/insurer for settlement.
Feedback/follow-ups:
In some cases, hospitals or the scheme portal may require feedback or documentation after treatment. Keep any discharge documents, bills, etc., even if they are submitted by the hospital.
Coverage and Benefits Of Bhamashah Swasthya Bima Yojana:
What the scheme provides, approximately:
- Cashless hospitalisation: For procedures/treatments included under the scheme in empanelled hospitals.
- Pre‑hospitalisation & post‑hospitalisation expenses: Usually 7 days before admission and 15 days after discharge are covered under the packages.
- Wide range of medical / surgical packages: Both secondary and tertiary care packages are included. The number of packages is large (over 1,400+ as per older info) including general illnesses, critical illnesses.
- Services in both government and private hospitals that are empanelled.
What Is Not Covered Under Bhamashah Swasthya Bima Yojana:
While the scheme is generous, there are some limitations:
- If a hospital is not empanelled, then a cashless facility may not be available. You may have to pay first and try to get reimbursement (if allowed) or might be outside scheme benefit.
- Eligibility criteria must be fulfilled: if someone is not in NFSA list or does not have required documents, the scheme benefit may not be available.
- Some packages / procedures may have specific rules / caps. Non‑covered treatments or items outside prescribed packages may not be paid for under scheme.
- Sometimes requirement to have taken ration from Fair Price Shop recently (i.e. active NFSA status) is needed. If you are NFSA but haven’t taken ration recently, eligibility may be questioned.
Steps for Availing Treatment Under Bhamashah Swasthya Bima Yojana:
Here is how you use the scheme when you need medical care:
- Identify a hospital empanelled under Bhamashah Swasthya Bima Yojana that offers the treatment you need.
- Go there with your Bhamashah card / Jan Aadhaar / Aadhaar / ration card and any other required IDs.
- On arrival, locate the help‑desk / Swasthya Sahayak / hospital staff responsible for Bhamashah Swasthya Bima Yojana processing.
- Present your details; let them verify you are an eligible beneficiary (NFS, A, etc.).
- If verification is successful, request admission/treatment as per the scheme terms. The hospital takes care of the cashless process for covered items.
- After discharge, ensure the hospital gives you all documents (discharge summary, bills, etc.), even if you didn’t pay; for your records.
FAQs:
Q. Do I need to apply separately for Bhamashah Swasthya Bima Yojana?
A. No, there isn’t always a separate application process in many cases. If you are eligible (under NFSA, have Bhamashah card, etc.), just going to an empanelled hospital with the required documents can enable you to access. But if your Bhamashah card / Jan Aadhaar or identity documents are not ready, you may need to complete those first.
Q. Can I get the Bhamashah card?
A. Yes. The Bhamashah card (or Jan Aadhaar slip / Bhamashah acknowledgement) is needed. If you don’t have one, you should register via the Rajasthan SSO portal or at local government / e‑Mitra centres.
Q. How long does it take to get the Bhamashah card/acknowledgement/enrollment?
A. In many cases, after documents are submitted, it may take a few weeks to a couple of months (commonly around 2‑3 months) for the card/acknowledgment/processing to be completed.
Q. Is the treatment really cashless?
A. Yes, for services/procedures that are covered under the scheme and if done at empanelled hospitals with verified eligibility, the treatment is meant to be cashless for covered items. However, if any procedure/item is outside what’s covered, or eligibility isn’t verified, you may have to pay for those.
Q. What if I go to a non‑empanelled hospital?
A. Cashless benefit likely won’t be available. You may have to pay out of pocket. The scheme is only valid at hospitals that are part of the Bhamashah Swasthya Bima Yojana network.
Q. How can I check if my name/family is listed under NFSA or the eligible list?
A. You can check via reports published by the Department of Food & Civil Supplies / NFSA, Fair Price Shop (FPS) lists, or visit grievance/help desks near you. Hospitals under the Bhamashah Swasthya Bima Yojana often check for you. Also, some government websites or portals may have searchable lists.
Q. How many medical packages/illnesses are covered?
A. The scheme covers a large number of hospitalisation packages/ailments. As per older data, over 1,400 packages/illnesses are included, spanning secondary and tertiary level care.
Q. Is there any waiting period after I enrol before I can use the scheme?
A. There is no confirmed public information that there is a long waiting period. But verification of eligibility (especially NFSA / ration card activity) might delay access. It’s advisable to complete documentation before an emergency arises.
Q. Are pre‑ and post‑hospitalisation expenses included? If yes, how many days?
A. Yes: the scheme includes 7 days of pre‑hospitalisation costs and 15 days of post‑hospitalisation costs around the event of hospitalisation.
Q. How do I find the empanelled hospitals under Bhamashah Swasthya Bima Yojana?
A. You can get lists from the health department of Rajasthan, district health offices, or from the official Bhamashah Swasthya Bima Yojana portal/state government’s health portal. Hospitals themselves usually display that they are empanelled. Also, the scheme’s manual/training material gives details.