Bone grafting remains a foundational procedure in orthopedics and dental medicine, providing crucial solutions for repairing bone defects and injuries. With increased life expectancies and more active lifestyles, the need for reliable bone regeneration methods has never been higher. Patients whose bones are compromised due to trauma, congenital disabilities, infections, or procedures such as tumor removal frequently require some form of grafting to restore function and stability.
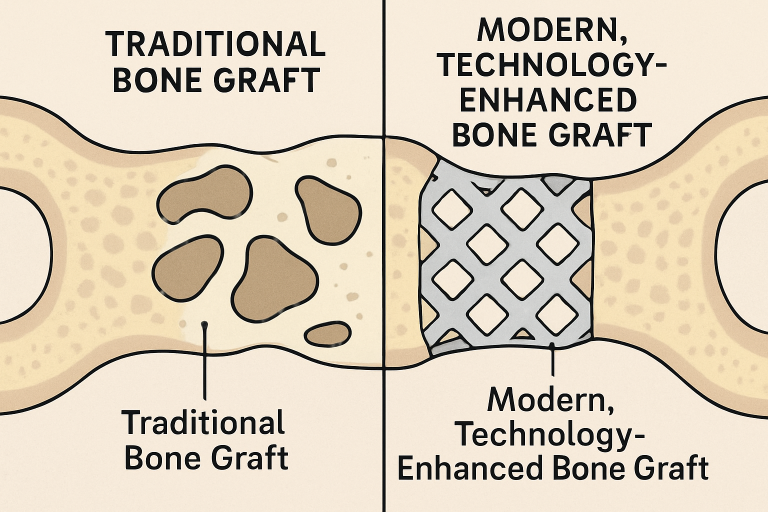
With rising patient demand for faster, safer, and more predictable results, cutting-edge research and technological advancements are rapidly transforming the landscape of bone regeneration. To address increasingly complex cases in modern care, clinicians are harnessing new tools—from highly customized implants to molecular-level materials—that push the boundaries of healing and integration. Today’s clinicians are looking well beyond the limitations of traditional autografts and allografts, increasingly integrating science and technology at a cellular or even atomic level to offer solutions that drive better outcomes.
For patients pursuing restorative treatments, particularly those considering a bone graft for dental implants, these advances mean improved outcomes and less invasive procedures than ever before. The ability to tailor treatments to each patient’s unique anatomical structure leads to greater satisfaction and empowers doctors with more options. From the dental chair to the operating room, the evolution of bone grafting is setting new standards for recovery time, durability, and patient comfort, paving the way for an era of truly personalized medicine.
3D-Printed Bone Grafts
Table of Contents
Integrating 3D printing in bone grafting is one of the most transformative technologies in recent years. By converting high-resolution imaging data from CT or MRI scans, personalized bone scaffolds can be precisely fabricated to fit the unique shape and size of the recipient’s defect. Unlike standardized, mass-produced grafts, these next-generation scaffolds replicate the exact anatomical contours of the target site, which is crucial for complex reconstructions or irregular injuries that do not fit ready-made solutions. This high degree of customization boosts the likelihood of graft success and ensures optimal contact between the graft and host tissue, supporting better load distribution and more stable healing environments.
In addition, novel printing materials, some of which are infused with bioactive compounds such as growth factors or antibiotics, support both the mechanical stability of the graft and the stimulation of natural bone growth. Advances in bioinks and printing methods mean that even living cells or blood vessel precursors can be integrated into printed grafts, raising the prospect of patient-specific, living bone implants.
The results are evident across both dental and orthopedic fields. Patients benefit from faster healing, reduced intraoperative adjustments, and a lower risk of graft rejection—a theme highlighted in The New York Times’ coverage of medical 3D printing breakthroughs. Surgeons experience greater precision during procedures with fewer complications, while the healthcare system benefits from lower costs due to reduced operative times and fewer revision surgeries.
Stem Cell-Based Therapies
Stem cell therapy is emerging as a promising frontier in bone regeneration. Unlike traditional graft materials, which rely on the patient’s natural healing abilities to populate a scaffold with new bone, stem cells introduce living, undifferentiated cells directly into the defect. These pluripotent or multipotent cells can transform into bone tissue, cartilage, or other supportive structures depending on local cues. Furthermore, stem cells secrete growth factors and cytokines that accelerate repair, enhance blood vessel formation, and support more robust bone formation.
For complex defects, avascular injuries, or cases with compromised bone quality, stem cell-enhanced grafts have been shown to improve healing rates and overall functionality significantly. These therapies are particularly compelling for older patients or those with medical conditions that impair healing.
Major research institutions continue to publish encouraging results, demonstrating stem cell therapy’s increased potential in clinical applications and offering hope for cases previously considered untreatable. As cell sourcing, preparation, and delivery techniques improve, the accessibility and consistency of these regenerative therapies are expected to grow rapidly.
Biomimetic Materials and Bioengineering
Bioengineers are designing next-generation materials that closely mimic human bone’s physical and chemical properties. These biomimetic scaffolds are often made from ceramics, composites, polymers, or hybrid structures, and are engineered to have the same porosity, mineral content, and microarchitecture as natural bone. This enables new bone cells to attach, proliferate, and thrive more effectively, combining the advantages of synthetic control with the natural cues necessary for effective repair.
Adding customized biological agents, such as bone morphogenetic proteins or gene therapy vectors, can further accelerate integration and regeneration. This combination of advanced scaffold design and molecular guidance makes it possible to address significant or irregular bone defects that were once unsolvable.
Exciting progress in this realm includes lab-grown bone tissues genetically identical to a patient’s bone, reducing immunological risks and postoperative complications. Scientists can now grow living bone outside the body using a patient’s cells, potentially providing a custom-fit biological implant that eliminates the risk of rejection. As these bioengineered constructs continue to advance, they may soon become viable options even for the most challenging reconstructive cases, such as craniofacial defects or significant trauma.
Minimally Invasive Techniques
The desire to minimize surgical trauma is driving a shift towards less-invasive bone grafting procedures. Traditional open bone grafting requires broad surgical site exposure, leading to longer surgeries, greater risks, and increased patient discomfort. In recent years, injectable bone grafts and endoscopic techniques have been developed to allow surgeons to introduce flowable materials or precisely shaped scaffolds through smaller incisions directly into bone defects.
These approaches significantly reduce the need for invasive surgery, enabling procedures to be performed with less anesthesia, shorter operative times, and lower risk of infection. Many minimally invasive grafting techniques can be performed in an outpatient setting, further reducing costs and improving efficiency.
Patients experience significant benefits, including less postoperative discomfort, reduced scarring, and faster recovery—all factors that enhance accessibility and satisfaction. These advances benefit dental implantology, pediatric patients, and individuals with underlying health issues. As these technologies evolve, they promise to bring bone grafting solutions within reach for a broader range of patients previously considered at higher risk for complications from surgery.
Nanotechnology in Bone Grafting
Nanotechnology enables researchers to manipulate materials at the molecular level, resulting in bone grafts that interact closely with existing bone tissue. Scientists can engineer graft materials’ surface structure, porosity, and chemical properties at the nanoscale, providing cues that guide cell behavior, increase cell adhesion, and enhance the release of growth factors. These precisely engineered nanoparticles can enhance the graft’s performance by improving cell signaling, accelerating mineralization, and promoting blood vessel growth within the healing area.
With enhanced bioactivity, nanomaterials are at the forefront of next-generation grafts that promise faster integration and superior biomechanical properties. Some approaches even include innovative materials that respond to changes in the healing environment by releasing drugs or adapting their mechanical properties to match the surrounding bone.
As this technology matures, we are likely to see bone grafts tailored for specific healing environments—whether pediatric, elderly, or for patients with underlying systemic conditions—further boosting safety and efficacy across diverse patient populations. The expanding role of nanotechnology is also poised to make bone grafts safer by minimizing infection risks and supporting the long-term stability of the implant.
Conclusion
The synergy between technology, biology, and engineering is redefining the future of bone grafting. Each year brings unprecedented advances in 3D printing, stem cell science, biomimetic materials, minimally invasive methods, and nanotechnology. Together, these technologies are converging to create faster, safer, and more predictable outcomes for patients requiring bone reconstruction. Continued investment and innovation will expand these benefits even further, making bone grafting a more successful and less daunting experience for patients worldwide, while empowering clinicians with more tools to deliver exceptional care.